Community health representative (CHR) Integration Tool No. 2
Vaccine deployment

This tool is intended for Tribal public health and community health representative (CHR) program leadership and teams as a best practice guide to ensure appropriate integration of CHRs into vaccine deployment efforts.
CHRs in vaccine deployment
The COVID-19 pandemic underscored the need for communities to prepare for public health emergencies, including vaccine deployment for infectious diseases. Tribally employed community health workers (CHWs), called community health representatives (CHRs), play a critical role in emergency response efforts and teams, serving as a vital link between official response agencies and local populations. CHRs are essential to comprehensive, equitable Tribal vaccine deployment plans and emergency response efforts due to their local expertise, trust-building capacity, cultural awareness, and ability to reach vulnerable groups.
Key roles
Risk communication
- They act as a critical link between the health system and the community to provide accurate and culturally competent messaging about response efforts.
Identification and support
- They provide information and services needed to ensure that socially vulnerable populations such as the elderly, the unhoused, and those with chronic illnesses get the help they need.
Health promotion and education
- They promote effective disease prevention and risk reduction strategies.
Data collection
- They gather health data as trusted members of their communities to guide equitable response and recovery strategies.
Logistical support
- They assist in the organization and distribution of essential supplies, including vaccines, PPE, food, and water.
COVID-19
During the COVID-19 pandemic, CHRs were highly involved in supporting the priority aims of the Indian Health Service’s Strategic Response(1).
Prevent
- Organized and carried out effective public education campaigns
- Delivered food, medication, and other essential supplies to vulnerable residents
- Supported and coordinated vaccination deployment
Detect
- Assisted with testing events and clinics
- Distributed home test kits
- Learned the signs and symptoms of disease
- Identified high-risk community members
Recover
- Assisted with the coordination of healthcare services (medical supplies, prescriptions, staffing) to support Tribal communities
- Shared best practices
- Supported individual and community resilience
Treat
- Monitored clients’ symptoms
- Supported the rapid referral of people who require hospitalization to appropriate services, including transportation
- Provided follow-up care and assessment
A national, unique, and impactful workforce
National workforce
The Indian Health Services (IHS) CHRs program was developed in 1968 and is the oldest federally funded community health worker workforce in the country. As a highly trained workforce with a nationally recognized scope of practice, more than 1,600 CHRs representing over 250 Tribes operate in all 12 IHS Areas.

Unique workforce
Community health representatives (CHRs) are unique from other health professionals because they are often members of the Tribal community that they serve, they speak the same language, and they have a deep understanding of the cultural and traditional knowledge of their clients. CHRs improve the social determinants of health and decrease health inequities in Tribal communities. Integrating CHRs in interdisciplinary health teams and interventions is an evidence-based practice. When involved, CHRs improve chronic disease prevention and management, mental health, and utilization and quality of healthcare.

Impact the social determinants of health
Social determinants of health are the conditions and factors outside of medical care that play a fundamental role in health and quality-of-life outcomes for a population.(2) As trusted, frontline community health workers, CHRs are highly engaged in activities that improve key social determinants of health, such as:
- access to health care
- social and cultural cohesion
- social justice
- environmental quality
- quality housing
- food access
These factors contribute to the health and well-being of individuals and the greater Tribal community.

Checklist resources
These checklists were adapted from “Checklist for Administrators, Managers, and Clinicians to Integrate Community Health Workers in Vaccine Outreach, Acceptance, and Distribution Strategies.” Prepared for the Association of Clinicians for the Underserved by the National Association of community health workers (2021).
Acknowledgments
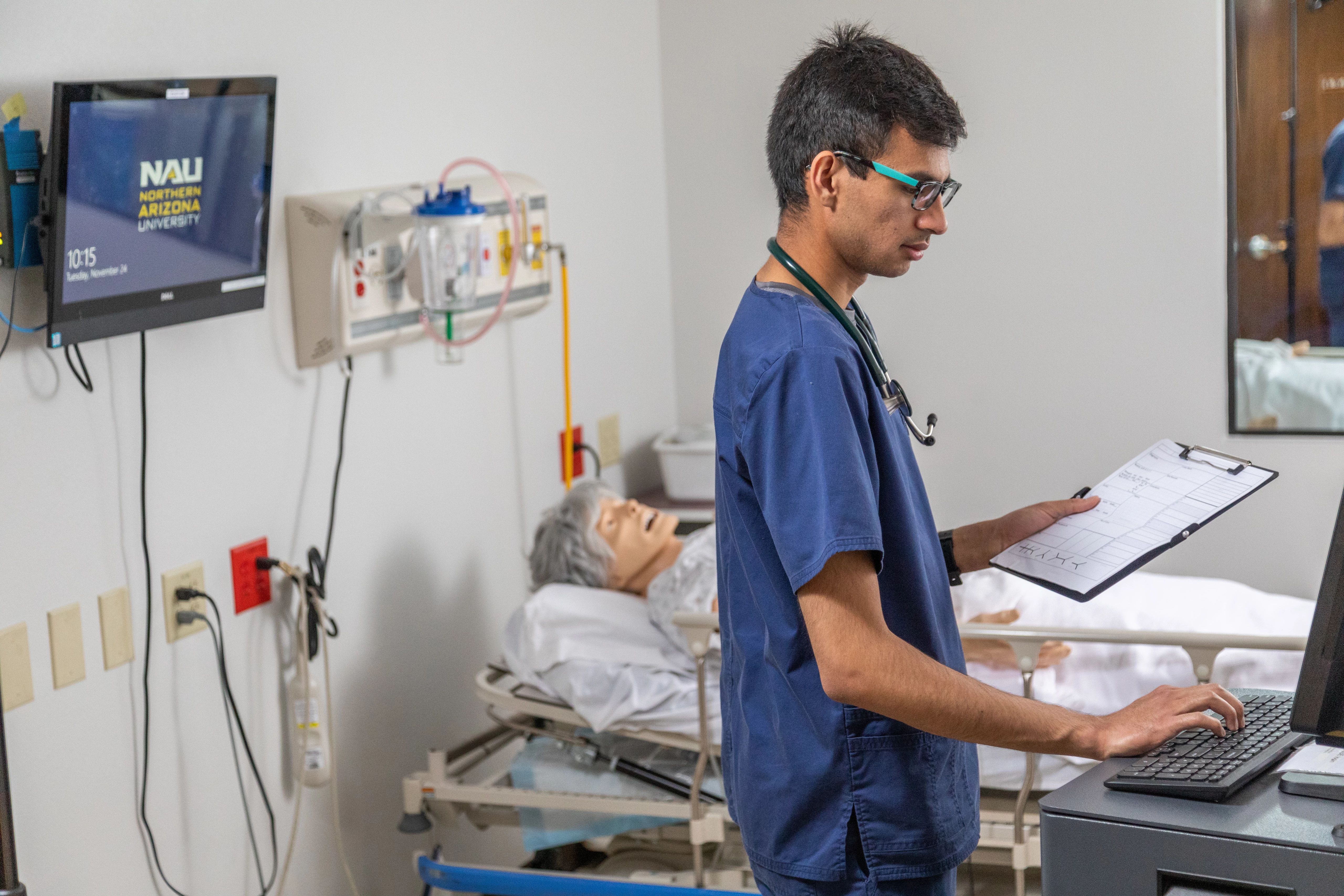
This guide was developed by the CHRs WITH uS! initiative (Community Health Representative Workforce Integration in Tribal Health Systems to Address COVID-19), which is a consortium of Arizona Community Health Representative Programs, the Arizona Advisory Council on Indian Health Care, and Northern Arizona University’s Center for Health Equity Research. These materials are informed by in-depth interviews with CHRs and managers, CHR program and Tribal emergency response plans and policies, and a literature review on CHR integration within public health emergency response plans and efforts. Photo credit: J. Daniel Hud.
Prepared by
- Northern Arizona University, Center for Health Equity Research
- Janet Yellowhair, MPH, Research Coordinator
- Louisa O’Meara, MPH, Research Coordinator Senior
- Samantha Sabo, DrPH, MPH, Professor Health Sciences
In collaboration with
- Brook Bender, Hualapai Tribe Senior Services Department
- Marianne Bennett, Salt River Pima-Maricopa Indian Community Community Health Services
- Fernando Flores Jr., Colorado River Indian Tribes Community Health Representative Program
- Joyce Hamilton, Hopi Tribe Department of Health and Human Services
- Rema Metts, Gila River Health Care Corporation Public Health Nursing
- J.T. Neva Nashio, White Mountain Apache Tribe Community Health Representative Program
- Sheryl Taylor, Cocopah Indian Tribe Tribal Health Maintenance Program
With review by
- Arizona Tribal Executive Committee, Public Health Emergency Preparedness
- Arizona Advisory Council on Indian Health Care, Tribal Pandemic Coalition Coordinator
- Indian Health Service Phoenix Area, Community Health Representative – Public Health Nursing Office
Endnotes
- IHS Covid-19 Response 100 Day Review. Indian Health Service. (2020) Accessed July 10, 2023.
- Office of Disease Prevention and Health Promotion. (n.d.). Social determinants of health. Healthy People 2030. U.S. Department of Health and Human Services.
- A Playbook for Local Health Departments to Advance CHW Engagement in COVID-19 Response Strategies. The Community-Based Workforce Alliance. (2021)
- CHR Standards of Practice. Indian Health Services. (1991)
- Resource Guide for Health Centers: Community Health Workers and COVID-19 Vaccine. MHP Salud. (2021)
- HIPAA Training and Resources. U.S. Department of Health and Human Services. (2023)
- Crisis and Emergency Risk Communication Training. Centers for Disease Control and Prevention. (2018)
- National Incident Management System (NIMS). Federal Emergency Management Agency (FEMA). (2015)
- National Preparedness Report: December 2022. Federal Emergency Management Agency (FEMA), National Preparedness Assessment Division. (2022)
Funding Acknowledgment: This publication was supported by the Centers for Disease Control and Prevention of the US Department of Health and Human Services (HHS) (NU58DP006992) Coronavirus Aid, Relief, and Economic Security Act (“CARES Act”) Public Law 116-136 Public Health Service Act 42 U.S.C. 301(a). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, CDC/HHS or the US Government.
