SHERC renewal features 3 projects focused on health equity
Investing in innovative research by early-stage investigators is an invaluable contribution of the Southwest Health Equity Research Collaborative (SHERC).

SHERC will fund three major research projects, led by researchers Ricky Camplain, Emily Cope, and Joseph Mihaljevic, that will improve health equity for people who are most underrepresented.
The projects are Camplain’s “Gender Differences in Physical Activity Opportunities and Impacts While Incarcerated”; Cope’s “Evaluation of Soluble Fiber as a Strategy to Decrease Asthma”; and Mihaljevic’s “Social-Spatial Clustering, Interconnection and Movement Analysis (SSCIMA): Integrating Analysis of Socio-economic Sub-population.”
“We are so fortunate to have such talented early-stage investigators as part of SHERC including these three researchers who are leading our main SHERC research projects for the next five years,” said Regents’ Professor Julie Baldwin, principal investigator for SHERC and director of the Center for Health Equity Research (CHER). “Drs. Camplain, Cope and Mihaljevic have all had SHERC pilot project funding previously and have now been successful in getting other NIH funding. All three are doing innovative research in areas that will make a difference for reducing health inequities for underrepresented and underserved populations in Arizona. We are so proud of their work and leadership.”
Examining gender differences in physical activity opportunities and impacts while incarcerated
Camplain, assistant professor for CHER and the Department of Health Sciences, is studying physical activity and sedentary behavior and their impacts on health outcomes among incarcerated women. The study’s long-term goal is to increase physical activity that improves physical and mental health in this population.

Each year, more than 9 million Americans are incarcerated in jail—facilities housing individuals awaiting trial and serving short sentences—with about 20 percent who are women, according to Camplain and co-investigators Heather Williamson, associate professor, Department of Occupational Therapy; Joe Mihaljevic, assistant professor, School of Informatics, Computing and Cyber Systems; Hendrik de Heer, professor, Department of Health Sciences; and Sara Shuman, assistant clinical professor, Department of Health Sciences.
Women incarcerated have more chronic conditions, psychiatric disorders, and drug dependence than men, according to the investigators.
“Women are often overlooked when planning for health and wellness in correctional settings because they make up a minority of the population. Physical activity can mitigate poor health outcomes and have immediate effects,” Camplain said. “A single bout of moderate-to-vigorous physical activity improves anxiety symptoms, decreases blood pressure, and improves sleep on the day it is performed. But we want to know if the jail environment is conducive for physical activity, not just among men.”
The research objective for their project is to determine gender disparities in physical activity opportunities in two co-ed county jails and examine the impact of these disparities on the health of women who are incarcerated, before and after release.
The research team will interview jail staff and individuals incarcerated to determine leisure and work-related physical activity opportunities and activities while incarcerated.
Over a year, they will recruit a cohort of a total of 500 men and women incarcerated at two northern Arizona jails to understand gender-based differences in patterns of time spent in physical activity and sedentary time while incarcerated and how those patterns impact physical and mental health during and after incarceration. Using data collected from the cohort, they will simulate realistic interventions that decrease sedentary behavior and increase physical activity to then share back with the jail facilities.
Dedicated to giving back to science and the community
The researchers will provide research results to the jails’ administration for recommended physical activity programming and policy changes. They hope their study raises awareness about the importance of community-engaged research with incarcerated individuals and encourages others to do research with communities impacted by the criminal justice system.
Evaluating soluble fiber as a strategy to decrease asthma
In Arizona, asthma prevalence exceeds the national average and is disproportionately seen in economically disadvantaged urban populations. Cope, associate professor, Department of Biological Sciences, and her co-investigators will study childhood asthma and the effect of the gut microbiome on improving asthma symptoms.
Co-investigators include J. Gregory Caporaso, professor, Department of Biological Sciences and director of the Center for Applied Microbiome Science in the Pathogen and Microbiome Institute; Andrew Koppisch, associate professor, Department of Chemistry and Biochemistry, and interim associate vice president for Research at NAU; and graduate student Kathryn Conn.
Matthew Rank, an immunologist and pediatrician at Mayo Clinic, will oversee the clinical trial and biospecimen collection at the Phoenix Children’s Hospital Pulmonary and Asthma clinic, which includes recruiting participants, assisting with data analysis, and interpretation as well as communicating the findings from the study to the public.
Sophia Williams, pediatric pulmonologist at Phoenix Children’s Hospital, will lead research performed on the Phoenix Children’s Hospital Breathmobile (a mobile asthma clinic) along with Ryan Sidebottom, family nurse practitioner, who will administer study questionnaires.
“We leverage a strong partnership between NAU and Phoenix Children’s Hospital to learn about the relationship between nutrition and asthma so we can address disparities in asthma across Arizona,” Cope and Rank said.
According to the investigators, asthma is a complex inflammatory disease of the airways that is estimated to affect 300 million people worldwide with an additional 100 million asthma diagnoses anticipated by the year 2025. Asthma is a multifactorial disease affected by genetic and environmental factors.
While asthma affects individuals across all income brackets and ethnicities, there is a significant disparity in occurrence, illness, and mortality among people living in low-income urban areas. In addition, the pediatric gut microbiome is critical in immune development and understanding childhood asthma may have lasting beneficial effects into adulthood, according to the investigators.
The scientists will measure fiber consumption and gut microbiome composition in patients who are served by the Breathmobile, and they will recruit participants from the Phoenix Children’s Hospital to determine if changing to a high-fiber diet through fiber supplementation can alter the airway and gut microbiome composition and lead to a decrease in asthma.
Dedicated to giving back to science and the community
According to the investigators, an essential part of their work is sharing the project’s results publicly with a community of scientists interested in gut microbiome research.
They plan to make all microbiome data available to the research community through deposition in publicly available databases and all software developed in this project will be published as open source. They will engage the community through the development of informational brochures as they gain knowledge about dietary habits and gut microbiota. They will also present their findings to the public during STEM (Science, Technology, Engineering, and Math) outreach events in Flagstaff (such as the Flagstaff Festival of Science) and Maricopa County.
Through their study, they will develop inter-institution collaborations and present their results at national scientific meetings and publications. In the future, they hope to focus on nutritional interventions for healthy food choices.
Using SSCIMA: Analyzing socioeconomic sub-populations to improve predictions of the spread of infectious disease
By the summer of 2020, serious health disparities associated with COVID-19 were becoming apparent. Nearly 50 percent of detected COVID-19 infections in Arizona were associated with the Latinx population and 13 percent were associated with the American Indian population, even though these populations make up only 31.7 percent and 3.9 percent of the overall population, respectively.
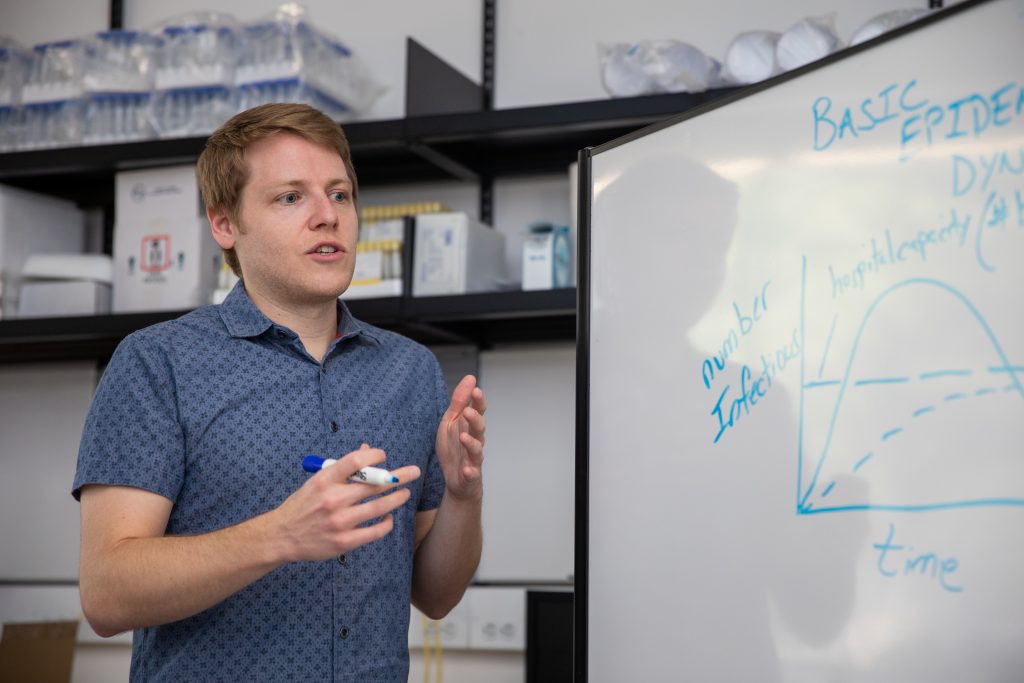
Through their SHERC project, Mihaljevic and his co-investigators are dedicated to addressing these health disparities by developing effective prediction models for infectious diseases, like COVID-19, that accurately examine small spatial scales that affect transmission rates and disease outcomes in local communities.
Mihaljevic is an assistant professor in the School of Informatics, Computing, and Cyber Systems, and his co-investigators include Eck Doerry, professor, School of Informatics, Computing and Cyber Systems and Ye Chen, assistant professor, Department of Mathematics and Statistics.
Their project aims are:
- Develop a geostatistical analysis method to discover “socio-spatially similar” sub-populations and quantify transmission linkages between them.
- Design algorithms that enable accurate and automated parameter estimation for complex epidemiological models.
- Engage community participation by developing outreach and educational elements.
“Our overall objective is to create better disease forecasts at spatial scales that are most relevant for decision-making [about the spread of COVID-19 or other pandemics]. We want models to be as accurate as possible so that public health stakeholders are empowered to use these model predictions in a useful way,” Mihaljevic said. “Moreover, we want these models to reflect the fact that populations differ in meaningful ways that can lead to health disparities. By bringing together experts in infectious disease, computer science, and mathematics, we hope to create usable and actionable technologies that will prepare us for future disease outbreaks.”
Their goal is to improve their spatial models to fit local disease data while also improving the accuracy of local forecasts. They also plan to eventually create software tools and outreach programs that will train new users to implement their disease modeling methods to respond to a variety of diseases.
Dedicated to giving back to science and the community
The team hopes to turn their technical developments into freely available software and to create an online testing bench for modelers.
To assist communities, they plan to develop a 90-minute, freely available webinar to build on the success of SHERC’s earlier Infectious Disease Epidemiology Bootcamp, which hosted a series of web-based modules that assisted with immediate public health workforce development during the COVID-19 pandemic.
The course will offer an introduction to epidemiological modeling, how to interpret common model outputs, and how to critically evaluate whether a model may or may not be relevant to some specific local context. They will also design an in-person half-day workshop to hold at academic conferences that train modelers to use our software package and online testing bench. It will include scenario-based training that demonstrates how to use our software to respond during a novel epidemic.
This research is supported by a NIMHD center grant to the Southwest Health Equity Research Collaborative at Northern Arizona University (U54MD012388).